Nutrition & Chronic Kidney Disease
Basic Kidney Diet Guidelines
Other Nutritional Concerns
Basic Kidney Diet Guidelines - Answers
Special thanks to Deborah Bethmann, RD, CDN, Renal Dietitian, for preparing the following information.
1. Why do I need to follow a special diet if I am on dialysis?
The healthy kidney takes out waste products and extra minerals from foods eaten. It keeps sodium and water balanced. It supports normal bone health by balancing phosphorus and calcium.
When your kidneys are not working properly they cannot get rid of waste products and extra fluids. Minerals in food eaten such as potassium, phosphorus, and sodium may also collect in your body which puts your heart, bones, lungs, and health at risk. The goal of the diet is to control your protein; potassium, phosphorus, calcium, sodium (salt), and fluid intake to help your dialysis treatments get rid of the waste products, minerals, and excess fluid.
In addition, your diet must give you enough calories and protein to support a healthy body. In addition, a dietitian will watch your nutritional status and develop a nutrition care plan based on your special and changing needs.
2. Should I increase or decrease my protein?
Protein is well known for its ability to build and repair body tissue. Adequate protein intake can help keep your immune system strong to defend your body against infections. However, when your body breaks down protein it produces waste products that build up in the blood and become harmful to the body. Healthy kidneys or an artificial kidney (dialysis) pull these waste products out of the body to prevent serious medical complications.
Eating a low protein diet before starting dialysis may help keep some kidney function and delay the start of dialysis. Your doctor will determine whether a low protein diet is good for you and refer you to a dietitian who can help plan your diet.
Once dialysis is started, protein and calorie needs are greater. Protein needs are increased but still need to be controlled. Not enough protein can cause muscle breakdown, weakness, and increase your chance of infection. Too much protein can create unpleasant symptoms such as nausea, vomiting, fatigue, and taste changes. Protein foods have high amounts of potassium and phosphorus, which are minerals that can remain in the body and reach dangerous levels. Your doctor and dietitian will decide your special protein needs and watch your laboratory values to adjust your diet as needed.
High quality protein foods (from soy and animal protein: chicken, fish, beef, eggs, dairy) are better absorbed by the body when compared to poor quality protein (from plant foods: bread, vegetable, beans). Animal protein can help you reach your best protein intake in smaller quantities than plant protein foods while reducing waste products, potassium, and phosphorus. To keep protein for it’s essential functions adequate calories must be eaten. You may achieve the best protein intake when you spread out your protein foods throughout the day instead of at just one or two meals. Your kidney doctor and dietitian will watch your protein needs and adjust your diet as needed.
3. What is potassium and why do I need to watch my intake?
Potassium is a mineral that is required by the body for nerve and muscle activity. It is found in all types of foods including meat, dairy products, dried beans, and is especially high in fruits and vegetables. When your kidneys no longer can filter extra potassium out of the body, it begins to build up in the blood endangering your heart muscle. Serious complications can occur with too much potassium in the body such as muscle breakdown, irregular heartbeat, and cardiac problems. Potassium levels can become too low and you may have muscle weakness, shakiness, and tingling feelings. You must maintain a good potassium level in the blood. Your doctor and dietitian will watch your potassium blood level and adjust your diet as needed.
Portion control (the amount of a food that you eat at one time) is essential in limiting the potassium content you eat. Boiled carrots provide 115 mg of potassium in ½ cup. If you eat 1 ½ cups of boiled carrots the potassium content will triple to 345 mg. This can also work towards your benefit. For example a high potassium tomato (1 small) provides 273 mg of potassium. If you cut a thin slice for your sandwich it provides much less; 1/6th of 1 small tomato provides 45 mg of potassium. Discuss your concerns and questions with your dietitian who may be able to teach you how to include some favorite foods. You may also learn ways to decrease the potassium in foods such as buying low sodium/sugar canned fruits and vegetables instead of fresh. Your dietician can also teach you how to double boil certain vegetables such as potatoes to lower the potassium content. You will be given a more detailed list and suggestions that are based on your dietary needs.
4. Why do I need to limit my phosphorus from food if I take phosphorus binders?
Your body likes to keep a balance between the two minerals - phosphorus and calcium - which are needed for bone health. A healthy kidney plays an important role in this balance by changing vitamin D to the active form, which helps the body to absorb more calcium if needed.
In kidney disease, the phosphorus in many foods may build up in the blood and upset this balance causing a decrease in blood calcium. This sets off an alarm in the body which signals a gland located in your neck to produce parathyroid hormone (PTH). Parathyroid hormone tells the kidneys to make active vitamin D to absorb more calcium. The diseased kidney can’t recognize this signal and it cannot make active vitamin D. The body continues to produce parathyroid hormone and the body begins to pull calcium from the bones, which is not good. Over time this can cause your bones to become brittle and easily broken, a condition referred to as "renal bone disease." The imbalance of phosphorus, calcium, vitamin D, and parathyroid hormone (PTH) levels can also cause increase hospitalizations and other serious complications including calcification or the hardening of arteries, joints, heart, skin, or lungs from calcium and phosphorus hard deposits, bone pain, and itching.
You can help prevent renal bone disease and other serious complications with the help from your renal care team by following these steps.
-
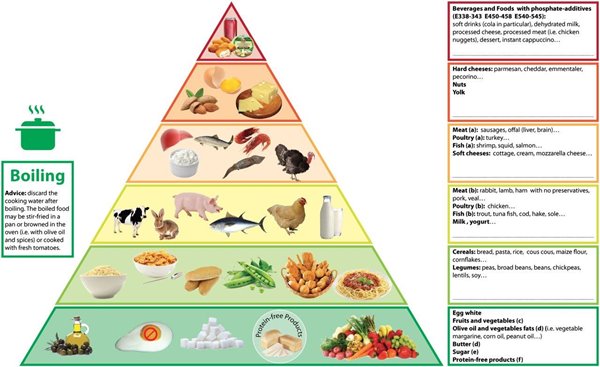
Eat a low phosphorus diet. Avoiding high phosphorus foods such as excess dairy foods - milk, cheese, yogurt, nuts/seeds, chocolate, beans, and bran. In addition avoiding foods that have phosphorus additives (hidden phosphorus) such as colas, muffin and pancake mix, processed meats - hotdogs, sausage, lunch meats, fast foods, and many processed and convenience foods. Read labels and look for ingredients similar to the word phosphorus such as dicalcium phosphate and phosphoric acid. Talk to your dietitian who can help you identify these foods. Phosphorus additives are absorbed by the body very well but do not bind well with your phosphorus pills. Since your body needs natural phosphorus sources from high protein foods such as beef, chicken, fish that bind well with your phosphorus binders, it is important that you choose these animal protein sources. Recent studies suggest that our bodies can't absorb phosphorus from plant proteins such as beans however beans are high in potassium so discuss with your dietitian before adding to your diet.
-
Good protein foods that you need to eat are often high in natural phosphorus therefore your doctor will prescribe a phosphorus binder for you to take with your meals and snacks. Phosphorus binders do exactly what the name says, they bind with phosphorus in foods since your body can no longer get rid of this excess phosphorus. There are many different types of phosphorus binders that are available as pills, chewable tablets, liquids, and powders that can be mixed in beverages. Take your phosphorus binders when you eat meals or snacks that contain phosphorus foods. Your dietitian will teach you how to adjust your phosphorus binders for the amount of phosphorus at your meals and snacks to achieve the most binding power. Make sure to take your phosphorus binders exactly how your kidney doctor and dietitian tell you. To work, phosphorus binders need to be taken with the meal, waiting 30 minutes or longer will reduce the binding power. They need to be taken with every meal and snack that contain phosphorus. Remember it is important to take the amount the doctor prescribed to you.
-
Your kidney doctor may prescribe additional medications. Your kidney care team of nurses, doctors, and dietitians will monitor your blood results for phosphorus, calcium, parathyroid hormone (PTH) levels, and often vitamin D. A "calcimimetic" medication that you take at home may be prescribed if your parathyroid hormone (PTH) levels are too high. Since the kidneys can not convert vitamin D to the active form; often the active form of vitamin D is given during your dialysis treatments or an oral form may be prescribed. Remember this is not the same vitamin D that you can get over the counter; although your doctor may prescribe this type of vitamin D too. It is important that you don't take over the counter vitamin D or calcium supplements before discussing with your doctor.
Your kidney care team will share your phosphorus, calcium, parathyroid hormone (PTH), and sometimes vitamin D blood results with you. This team will make sure you know what you need to do to keep these levels in the best target ranges. Remember to get your phosphorus from the best sources - protein foods and watch out for those hidden phosphorus sources. Your dietitian will teach you the best phosphorus foods for you to choose, limit, or avoid. Your dietitian will also make sure you know how to take your phosphorus binders and any other medications your doctor prescribes for phosphorus, calcium, and parathyroid hormone control.
5. Why do I need to limit my sodium and fluids?
One of the important functions of the healthy kidney is its ability to regulate sodium (salt) and water (fluid) balance. The kidneys will keep sodium or fluids if body amounts become too low. They will rid the body of extra fluids or salt to keep the body’s proper balance. This balance of salt and fluid helps to control blood pressure.
When your kidneys are not working sodium and water are not in balance. High salt intake can start the body's thirst reaction, which will lead you to drink more water. In kidney disease this natural response to drink more may cause your body to swell and gain weight, often called edema. Your heart may become enlarged as it works harder to pump blood with the excess fluid weight. You may experience shortness of breath and high blood pressure.
Reducing your intake of high salt foods and controlling your water intake is essential. Putting down the salt shaker is not enough. You will need to reduce your intake of high salt foods such as canned foods, frozen dinners, olives, soy sauce, deli-style lunch meats, cheese, canned soups, and packaged food items. Many restaurants offer healthier choices, so call ahead to see if low salt items are on the menu. Talk to your dietitian to learn which foods you’ll need to reduce and how to read food labels for salt content. You may be surprised to learn how much salt is in some foods.
Keep track of the fluids you drink and remember to count any food item that melts at room temperature such as sherbet, Jell-O, and ice cubes. Drain all liquids from canned fruits and low salt vegetables. Count on water as being a true thirst quencher instead of sodas or sugar-containing drinks. Try to learn from past mistakes. If you gain too much fluid weight, look back at the previous days and try to find out why the fluid gain happened. Did you have a high salt meal? Did you lose track of your fluid intake when at a family party? Talk with your dietitian who may be able to offer help in finding answers for these problem areas.
Other Nutritional Concerns - Answers
1. How do I make all these changes in my diet with everything happening at one time?
-
Making changes in your eating habits is not easy. You may feel frustrated, overwhelmed, and angry. It is even scary to change old familiar habits for new ones. The following tips may help you with the needed changes in your diet.
-
Recognize that your feelings of frustration, fear, and/or anger are normal. Discuss these feelings with your social worker and/or dietitian.
-
Learn why the changes are needed.
-
Think positive - what foods can you have instead of what foods you can’t have.
-
Try to develop motivational factors to help you approach the changes. Such as, "This is an area of my treatment I can help control", or "I want to keep my heart, bones, and body strong so I can feel better."
-
Discuss favorite foods with your dietitian, who may be able to teach you moderation techniques to fit some forbidden foods back into your diet.
-
Discuss any concerns or problems with your team of doctor, nurses, dietitian, and social worker to help you with additional strategies.
2. What if I don’t have an appetite?
People new to dialysis often complain of a poor appetite. This may be explained in part by recent hospitalization and illness. Emotional feelings prior to and when starting dialysis can also affect one’s appetite. The build up of waste products can cause taste changes, nausea, and vomiting and will affect the desire to eat. Once dialysis begins and the amount of waste products in the blood is lowered, appetite may improve.
-
Remember it is important to discuss any appetite changes with your dietitian who can give you specific suggestions based on your own needs. The following tips may be useful if you do not feel like eating:
-
Remember the effect that good nutrition has on your general health. Poor nutrition can weaken the immune system and make you more likely to get an infection or other illness.
-
If large meals are overwhelming, try eating smaller meals or snacks more frequently.
-
Make smaller portions of food mean something. Raise the calories by adding nutrient dense sugar and fat to your food. If you have diabetes, discuss with your dietitian how to fit sugar in your diet.
-
Your dietitian or doctor may recommend a nutrition drink or supplement. Products have been developed for kidney patients and their special needs.
-
Have already prepared foods and snacks on hand. You may find it easier to eat when food is already prepared instead of having to make it.
-
Talk to your dietitian who may be able to provide you with additional tips to ensure adequate nutrition.
3. My cholesterol is high; do I need to be concerned?
Heart disease is a serious concern for the kidney patient. In addition to replacing folic acid, a water -soluble vitamin that can be depleted during dialysis, a low cholesterol and saturated fat diet may help prevent this disease. However, whether it is appropriate for you to follow a low cholesterol, low saturated fat diet is dependent on many factors including your doctor’s recommendations, current and past medical history, willingness to make additional changes, and your nutritional status.
Fat is an important calorie source for you. Starting a low cholesterol and low saturated fat diet may cause weight loss if calories are not replaced by other sources. Weight loss may or may not be beneficial depending on your nutritional status. Malnutrition with low body weight and low protein is a major concern for you. A cholesterol restriction may not be appropriate for an elderly or malnourished patient when it is crucial that adequate nutrition is achieved and/or maintained. Cholesterol and saturated fats may improve the taste of foods and therefore contribute to increasing one's appetite and protein intake. Your dietitian may assess your cholesterol value to determine whether you are eating well or poorly.
The following suggestions may be beneficial if low cholesterol and low saturated fat restrictions are needed.
-
Replace unhealthy saturated fats with heart healthy monounsaturated fats found in canola and olive oils. Polyunsaturated fats such as safflower, sunflower, and corn oil may also be used. In addition, omega 3 fatty acids found in fatty fish such as salmon and mackerel may be eaten. Monounsaturated and polyunsaturated fats are also good calorie boosters if weight gain or preventing weight loss is a goal.
-
You may need to limit egg yolks to 3-4 per week but continue to eat the egg whites for protein or replace your eggs with cholesterol-free egg substitutes.
-
Choose lean cuts of meat and trim the excess fat.
-
Replace butter with soft margarine or even better olive or canola oil.
-
Bake, poach, steam, stir fry, and roast instead of frying.
-
Choose low fat items such as non-fat milk versus whole milk.
4. What about my diabetes?
Many people with diabetes have been taught to eat more foods with fiber, to limit protein intake, and limit total fat intake. These recommendations were fine before kidney disease was found; some changes may need to be made by those on hemodialysis. Foods high in fiber such as fruits, vegetables, beans, and bran/whole grains need to be limited or avoided because of their high potassium and phosphorus content. Protein needs are often higher because of losses that occur during the dialysis procedure. In some people with kidney disease, fat may become an important calorie source that helps fight weight loss.
A poor appetite, which leads to weight loss and malnutrition, may increase your need for concentrated sources of calories such as fat and sugar. Maintaining carbohydrate intake at meals (often difficult with a poor intake) is essential if insulin is used. If a person with kidney disease and diabetes is not eating sufficient calories and carbohydrates then sugar may be beneficial. Talk to your dietitian before adding additional sugar.
Carbohydrate counting is a new method to teach diabetes control. It controls total carbohydrate intake from starches (breads, pasta, cereal, rice), fruits, milk, and sugar. The new recommendations include sugar, sweets, and desserts used in moderation and often replacing another carbohydrate source. Using sweets in moderation can be a nice treat with so many diet restrictions but the key word is moderation. Foods high in sugar or sweets will use up a lot of your daily carbohydrate allowance and they most likely will be lacking in essential vitamins and minerals. Talk to your dietitian if you would like to learn more about carbohydrate counting and using foods with sugar in your diet.
Regular meals, snacks eaten at the same time, use of the same kind and amount of food is useful to regulate blood sugar levels, especially if insulin is used. Skipping meals or scheduled snacks when using insulin can cause low blood sugar levels with symptoms such as shakiness, confusion, blurred vision, and sweating. People with diabetes are often taught to grab some orange juice when a low blood sugar reaction occurs. Most people with kidney disease must limit or avoid orange juice because of the potassium content and must learn appropriate food items to consume during a low blood sugar reaction. Using cranberry juice or glucose tablets are better substitutes.
5. What if I get a transplant?
Your kidney care team will guide you to make the right food choices based on your needs after your transplant.
6. Examples of Foods High in Potassium
Food item potassium content (in mg)
-
1 medium orange; 250 mg
-
1 medium raw avocado; 1097 mg
-
½ cup baked beans; 455 mg
-
½ cup boiled spinach; 419 mg
-
1 baked sweet potato with skin; 397 mg
7. Examples of Foods Low in Potassium
Food item potassium content (in mg)
-
½ cup unsweetened applesauce; 91 mg
-
½ cup blueberries; 65 mg
-
½ cup canned no salt added green beans; 78 mg
-
½ cup frozen and boiled carrots; 115 mg
-
1 slice white bread; 27 mg
List of High Potassium Fruits and Vegetables
-
nectarine
-
cantaloupe
-
honeydew melon
-
fresh pear
-
dried fruit
-
dates
-
raisins
-
dried figs
-
mango
-
kiwifruit
-
orange
-
prunes
-
pomegranate
-
plantain
-
apricots
-
avocados
-
artichoke
-
kohlrabi
-
fresh mushrooms
-
chili pepper
-
rutabagas
-
tomato
-
okra
-
cooked spinach
-
acorn squash
-
swiss chard
-
potatoes
-
beet greens
-
baked beans
-
pumpkin
-
butternut squash
-
collard greens
-
succotash
-
dried peas
-
lentils
-
beans (black, kidney, red)
8. Potassium Content of Certain Vegetables
(1/2 cup or 1 small piece = 200 –350 mg of potassium)
artichoke, kohlrabi, fresh mushrooms, chili peppers, rutabaga, cooked spinach, tomato (sauce & juice), okra, acorn squash, french fries, swiss chard, beet greens, sweet potato, baked beans, butternut squash, pumpkin, collard greens, parsnips, brussel sprouts, potato, swiss chard, succotash, dried peas & beans, lentils
9. Potassium Content of Miscellaneous Foods
Food item/serving size; potassium content (in mg)
-
12 ounces beer; 111 mg
-
4 ounces red wine; 145 mg
-
6 ounces brewed coffee; 96 mg
-
1 ½ ounce milk chocolate bar; 169 mg
-
1 packaged prepared oatmeal; 100 mg
-
½ cup bran cereal; 354 mg
-
1-ounce potato chips; 361 mg
-
1 slice pumpernickel bread; 139 mg
-
6 ounces yogurt; 400 mg
-
1 tablespoon molasses; 293 mg
-
1 ounce dry roasted cashews; 160 mg
-
1 ounce toasted sunflower seeds; 139 mg
-
¼ teaspoon (potassium containing) salt substitutes; varies from 50–650 mg
10. Foods High in Phosphorus
If you already looked at the list of high potassium foods, you may see a similarity in the following list. High potassium foods are typically also high in phosphorus. Take note, 3 ounces of animal protein from meat, fish, or chicken can provide almost 200 mg of phosphorus. Remember it is important that you eat the right portion size of animal protein foods to ensure adequate nutrition but not exceed your phosphorus restriction. Your dietitian will teach you the proper serving size of animal protein foods you require to meet your unique needs.
Some food items listed below may not seem so high in phosphorus. For example, 12 ounces of cola beverage contributes 50 mg of phosphorus. However this really can add to your total daily phosphorus intake and not leave room for essential food items such as animal protein foods. Compare cola to a similar food item such as 12 ounces of cream soda, which won’t contribute any phosphorus.
Food item/serving size; phosphorus content (in mg)
-
½ cup dairy (milk, yogurt, pudding); 110 mg
-
1 waffle from mix; 257 mg
-
1 large pancake from batter; 191 mg
-
12 ounce beer; 147 mg
-
12 ounce cola; 50 mg
-
9 pieces of caramel candies; 81 mg
-
½ ounce milk chocolate bar; 95 mg
-
1 packaged oatmeal; 133 mg
-
½ cup bran cereal; 344 mg
-
1 ounce cheese; 100 – 175 mg
-
½ cup vanilla ice cream; 70 mg
-
1 slice pumpernickel bread; 70 mg
-
1 slice whole wheat bread; 65 mg
-
½ cup chickpeas; 216 mg

